IBS is a Functional Gastrointestinal Disorder or Disorder of Gut-Brain Interaction?
Functional GI Disorder is one where there are no structural abnormalities in the gut seen on x-ray, endoscopy or blood tests, but functionally, the gut’s movement is abnormal. The Rome IV ((1)) update describes IBS as a disorder of gut-brain interaction. This is a further advance from calling IBS a functional GI disorder.
Defining IBS as a disorder of gut-brain interaction has been a remarkable advance in our perception of the condition. Many of you have been told “It is stress” or ” It is all in your head”, which somehow implies that it is within your control. Sometimes well-meaning friends and relatives make things worse by suggesting that all you have to do is “think positive”! I am not suggesting that you shouldn’t “think positive” but I haven’t met anyone who deliberately thinks negative thoughts! 🙂
IBS is a condition much like high blood pressure or diabetes and therefore needs to be addressed appropriately.
Gut-Brain Interaction
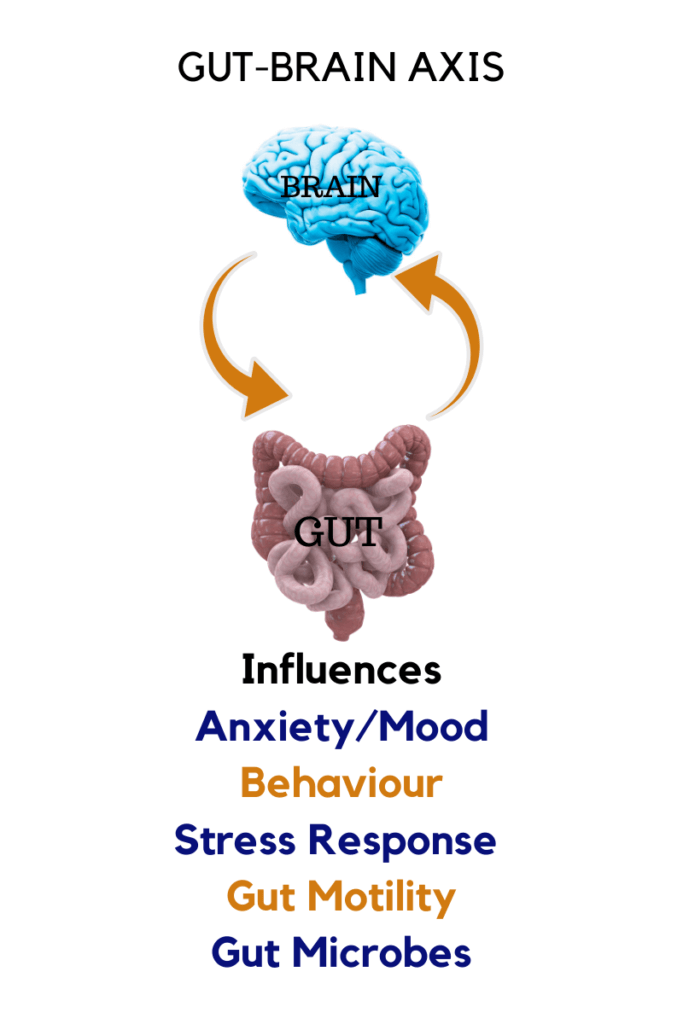
Your gut and the brain are constantly communicating with each other. We have always considered the brain to be the master controller of body functions. Animal and human studies in the last few years have shown that the gut controls the brain as well! The signaling between the gut and brain is bi-directional. In fact, the gut is called the “second brain”. However, this brain is not the part of you that composes great music or writes prose, but the part important for gut function, interaction with gut microbes, secreting neurotransmitters and many more.
In fact, the gut is primary and therefore IBS is called a disorder of gut-brain interaction and not brain-gut interaction.
There is a complex nervous system in the gut called the Enteric Nervous System (ENS). The ENS communicates with the brain through nerves called vagus nerves.
Symptoms Of IBS
| SYMPTOMS OF IBS |
| Recurrent abdominal (stomach) pain. Dull aching diffuse pain, commonly in the lower abdomen. Sometimes acute pain in addition to dull pain. |
| Pain relieved by defecation (passing stools) |
| Feeling of incomplete evacuation |
| Food may sometimes worsen the pain |
| Bloating or distention or “gassy” feeling |
| Passage of mucus |
| Constipation |
| Diarrhoea |
| Constipation alternating with diarrhoea |
Causes Of IBS
The exact cause of IBS is not known but different factors are relevant to the condition:
- Altered pain perception. People with IBS have been found to have a higher sensitivity to pain sensations, particularly pain related to distension of the gut.
- Disturbed immune function in the gut lining (mucosa)
- Gut dysbiosis- Imbalance of gut bacteria.
- Increased intestinal permeability (leaky gut)
- Low-grade inflammation
- Psychosocial disturbance, Adverse Childhood Experiences (High ACE Score)
How Is IBS Diagnosed?
Diagnosis is commonly based on symptoms after diseases like IBD, celiac disease, colon cancer or post-infectious malabsorption have been ruled out.
What are the criteria for diagnosis :
Recurrent abdominal pain on average at least 1 day/week in the last 3 months. These criteria should be fulfilled for the last 3 months with symptoms starting at least 6 months before diagnosis, associated with two or more of the following:((2))
| 1) Related to defecation |
| 2) Associated with a change in the frequency of stool |
| 3) Associated with a change in the form (appearance) of stool |
Some Important Facts About IBS
- IBS is distinct from IBD (Inflammatory Bowel Disease, like Ulcerative Colitis and Crohn’s Disease). IBD are autoimmune diseases causing specific conditions in the intestine. (One type of IBS is autoimmune).
- Constipation may result in complaints of hard stools or infrequent motions.
- Often constipation may not respond to regular laxatives.
- Diarrhea may mean frequent passage of small volumes of loose stools.
- Needing to use the toilet soon after a meal may be common.
- Constipation or diarrhea may be a predominant feature, but sometimes the symptoms may be mixed.
- IBS can occur after a gastrointestinal infection with a bacteria, virus or parasite–post-infection IBS.
- Though IBS is strictly not an infectious disease, microscopic inflammation has been detected in some people.
- Food intolerances may have symptoms similar to IBS.
- Early life stressors (High Adverse Childhood Experiences Score) is related to IBS.
Types of IBS
IBS is usually described as the following different types based on symptoms. The different types may change over a period of time. You may start off with IBS-D and later have a mixed type, IBS-M, and so on.
- IBS-D -Diarrhoea predominant
- IBS-C-Constipation predominant
- IBS-M-mixed constipation and diarrhea
- IBS-U-Unclassified
Other Conditions Associated With IBS
Besides the common symptoms of IBS, which are abdominal (stomach) pain, bloating, diarrhea and/or constipation there may be other associated conditions like
- Fibromyalgia
- Sexual dysfunction including poor libido
- Urinary complaints, Interstitial Cystitis
- Mucus discharge from the anus.
- Restless-leg syndrome
Danger Signals: When Is It Unlikely To Be IBS?
If you have any of the features listed below, it is important to rule out other organic diseases. You need to meet a well-qualified physician to help you with this.
- Passing blood with stools which is not caused by piles or anal fissures.
- Unintended weight loss of >10% of body weight in 3 months.
- Sudden or progressive changes in your symptoms.
- Fever
- Family history of Inflammatory Bowel Disease (IBD), celiac disease or colon cancer.
- Your symptoms wake you up at night.
- Your symptoms started for the first time after the age of 50 years.
Subsequent posts will cover dietary approaches, mind-body intervention, probiotics.


