Patient story: A 59-year-old woman has diabetes for 20 years with early kidney damage, presently on insulin injections. She had an angioplasty nine years ago because of chest pain from blocked heart arteries. Besides insulin, she was taking Plavix (Clopidogrel) and Nexium (PPI). Plavix works on blood cells called platelets to prevent them from sticking […]
Should You Stop Eating Gluten-Containing Food?
(An earlier version was posted in April 2019. Updated November 2019) What Is Gluten? Gluten is a family of proteins found in grains like wheat, spelt, rye and barley. It consists of two main proteins, glutenin and gliadin. Gluten is the component of grains that helps them bind together, like when you roll out a […]
Mind-Body Interventions In Irritable Bowel Syndrome (IBS):
Irritable bowel syndrome (IBS) is a disorder of gut-brain interaction, which produces symptoms of abdominal pain and change in bowel habits in the absence of organic disease. What are the Mind-Body Interventions? The National Centre for Complementary and Integrative Health, USA defines mind-body interventions as those practices that “employ a variety of techniques designed to facilitate the mind’s […]
Is “Leaky Gut” Affecting Your Health?
Many of you tell me that you have “Leaky Gut Syndrome”. What does this mean? Internet definitions of “Leaky Gut Syndrome” have described it as a condition where your gut lining works like a sieve and allows bacteria and other toxins to pass into the bloodstream and causes symptoms like bloating, fatigue, etcetera. However, a […]
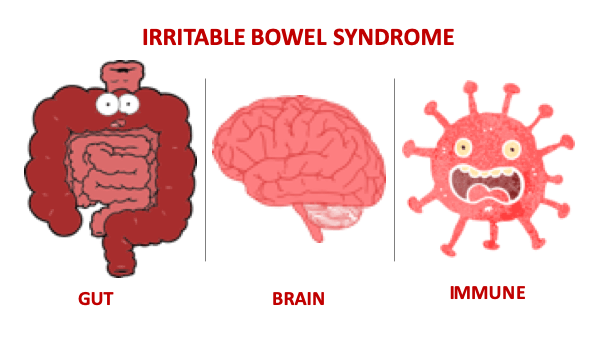
What Is Irritable Bowel Syndrome (IBS)?
IBS is a Functional Gastrointestinal Disorder or Disorder of Gut-Brain Interaction? Functional GI Disorder is one where there are no structural abnormalities in the gut seen on x-ray, endoscopy or blood tests, but functionally, the gut’s movement is abnormal. The Rome IV ((1)) update describes IBS as a disorder of gut-brain interaction. This is a […]