Many of you tell me that you have “Leaky Gut Syndrome”. What does this mean?
Internet definitions of “Leaky Gut Syndrome” have described it as a condition where your gut lining works like a sieve and allows bacteria and other toxins to pass into the bloodstream and causes symptoms like bloating, fatigue, etcetera. However, a medical definition of the syndrome is a combination of symptoms resulting from a single cause or commonly occurring together so as to fit a distinct clinical picture. Herein lies the problem!
“Leaky gut syndrome” is not recognized by the established medical community as a specific disease.
It is not listed as a diagnosis in the International Classification of Disease and this is why many of you may have been told by your doctor that you should stop looking for information on the internet! 🙂 However, scientific studies have shown enough evidence to make it an intriguing field of study.
“Leaky gut” or Increased Intestinal Permeability?
“Leaky gut” is essentially another way of describing increased intestinal permeability or impaired gut barrier function. But whether it can be called a “syndrome” as defined in medicine, is definitely open to debate! 🙂
Your gut is lined by cells that are closely connected to each other by tight junctions (TJs). This layer keeps the “baddies” away from areas where they can cause mayhem. This layer is not like a concrete wall that prevents all substances from going across. The tight junctions are extremely dynamic and highly regulated so as to maintain normal permeability. Healthy TJs make sure that harmful substances that affect your immune system are kept away while allowing the normal passage of electrolytes, nutrients, and water.
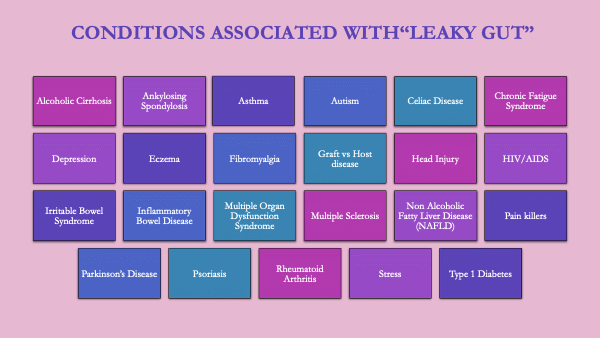
Abnormal gut permeability has been associated with several diseases.((1)) In the image shown below, you can see that some of these conditions are autoimmune, while others are not.
Gut Barrier Dysfunction And Autoimmunity
The gut barrier has a very important function of controlling the flow of substances (antigens) that can trigger an immune reaction. Thus the tight junctions in the gut are very important in controlling tolerance and autoimmunity.
Dr.Alessio Fasano, a Pediatric Gastroenterologist discovered Zonulin, ((2)) which plays an important role in controlling the function of tight junctions in the gut lining. An autoimmune condition develops when this zonulin pathway is disrupted in those who have the genes for autoimmune disease. Therefore 4 things have to be present at the same time for you to develop an autoimmune disease. These are:
- Genes
- Immune dysfunction
- Gut Barrier Dysfunction
- Presence of a trigger.
All four factors have been identified clearly in celiac disease. The genes are HLA DQ2 and DQ8, antibodies are produced against gluten in wheat (trigger) and there is increased permeability of the gut barrier. In other autoimmune conditions, while the genes are known and several antibodies have been identified, the trigger may not be as specific as it is in celiac disease. (Triggers of autoimmunity will be covered in other posts).
Are There Specific “Symptoms of Leaky Gut”?
Many of you have come to me suggesting that you have “symptoms of leaky gut”. What are some of those symptoms that you think are from “leaky gut”? Bloating, fatigue, headache, diarrhea, constipation, joint pain and many more. As you can read from this list, the symptoms are non-specific and overlap between many conditions like IBS, or non-celiac gluten sensitivity (link). Therefore, there are no specific symptoms of “leaky gut” ( and hence no magic pills to treat this! :-))
How Is Increased Intestinal Permeability Diagnosed?
If you have an autoimmune condition, you can assume that you have increased intestinal permeability, even without testing.
Many of you are always looking for the “latest test” (or latest magic supplement!) but
Is it worthwhile testing for increased gut permeability?
The tests available varies in different parts of the world. The commonest test is the
Lactulose-mannitol Test: In this test urinary sugars are measured after consuming lactulose and mannitol. This test is not 100 percent reliable because in some cases people with celiac disease have tested normal ((3))on this test.
Serum Zonulin Test: As mentioned above, zonulin is very important in controlling the tight junctions in the gut. Therefore high levels of zonulin may indicate higher gut permeability. However, it is not absolutely reliable ((4)). Moreover, zonulin levels may be high in other conditions like high blood pressure ((5))and prediabetes.
Treatment
Treating the underlying disease is the most important first step. This starts with the basic steps of SEMMT outlined in my eBook
What Else Can You Do? Things to avoid/reduce:
- Gluten: Withdrawal of gluten is the specific treatment for celiac disease, but gluten sensitivity is associated with several other conditions as well. (Nonceliac gluten sensitivity). Gluten withdrawal ((6))reduces gut permeability in celiac disease, and this may be true in other conditions ((7))as well. Most of the benefits of gluten withdrawal may be through effects on the gut microbiota.
- Food Additives: Use of industrial food additives ((8)) like glucose, salt, emulsifiers, organic solvents, gluten, microbial transglutaminase have been associated with increased gut permeability.
- Proton-pump Inhibitors (PPIs): PPIs are drugs like omeprazole, lansoprazole, esomeprazole are some of the commonest drugs prescribed today. They are usually prescribed for dyspepsia, reflux or pain killers. As this study shows, PPIs have the potential to increase gut permeability. ((9))
- PPIs and painkillers together may be worse: Many of you are prescribed a PPI with painkillers (NSAIDS). While it may save you from stomach ulceration, it may be quite the opposite for your small intestine ((10))
- Fructose: Fructose is a sugar, present in table sugar, fruits, honey and is used as an additive in food processing. Fructose is like a “stealth bomber”. It does not increase your blood glucose or insulin levels but goes directly into the liver and messes up your metabolism. One of the pathways is through affecting gut permeability. ((11))
- Alcohol: Besides the known adverse effects of excessive alcohol consumption, it is also associated with increased intestinal permeability. ((12))
- Stress: We know that if you don’t manage your stress well you will be unhealthy. Increasing gut permeability is one more pathway that stress impacts adversely.((13))
What Else Can You Do? Things To Add
- Probiotics
- Vitamin D3
- Glutamine
- Zinc
Probiotics:
Probiotics are defined as “live microorganisms that, when administered in adequate amounts, confer a health benefit on the host”(FAO/WHO). The important point to note is “when administered in adequate amounts“. Several studies have shown the benefits of using probiotics in affecting gut permeability.((14)) ((15))
What should you look for in a probiotic:
The minimal requirements for an effective probiotic are the following
1. That microbes must be alive in an adequate number when administered.
2. Strains must be identified genetically, classified using the latest terminology, and designated by numbers, letters, or names.
3. Appropriately sized and designed studies must be performed to designate a strain as probiotic and using the strain(s) on the host to which the probiotics are intended (human, livestock, companion animal, etc).
4. Strains shown to confer a benefit for one condition may not be probiotic for another application.
5. Strains that are probiotic for humans but are being used in animal studies should be clearly designated as human probiotics under experimental testing.
6 . Fermented foods, prebiotics, fecal microbiota transplant, and microbial strains of the same genus or species as documented probiotic strains but have not undergone appropriate testing on the target host should not be considered as probiotics.
Quoted from the reference. ((16))
Vitamin D:
Vitamin D is important for maintaining gut and immune system function. In a study of patients with Crohn’s disease, vitamin D 3 at 2000 IU/day for 3 months reduced inflammation and helped gut permeability. Those achieving blood vitamin D3 levels of ≥ 75 nmol/L (30 ng/dl) showed better benefits. ((17))
Glutamine:
Oral glutamine ((18)) and whey protein both reduced gut permeability in patients with Crohn’s disease. However, an older study ((19))showed no benefits of oral glutamine at 7 grams a day for 4 weeks. Glutamine is taken intravenously ((20))has shown a reduction in gut permeability.
Zinc:
Zinc is an essential nutrient involved with approximately 100 enzyme actions and plays a role in immune function and wound healing. It is also required for a proper sense of taste and smell. In a study ((21))on cells in a petri dish zinc deficiency showed increased membrane permeability.
Summary
- “Leaky Gut” and increased intestinal permeability are the same conditions.
- It is doubtful if there a specific “syndrome of leaky gut”.
- The purported symptoms of the syndrome are non-specific and common to other conditions as well.
- Several diseases and conditions are associated with increased gut permeability.
- Gut barrier dysfunction is a key process in autoimmunity.
- Is it necessary to test for gut permeability?
- Treating the underlying disease rather than merely treating symptoms leads to long term health.


