Prevention of depressive symptoms –this is not an expression we often hear. But this is what a clinical study decided to find out. The menopausal transition can be challenging for many women, both physically and emotionally. One of the most common symptoms that women may experience during this time is depression.
What is menopause?
Menopause is a natural biological process that marks the end of a woman’s reproductive years. It occurs when a woman’s ovaries permanently stop producing eggs, and her menstrual cycles stop. You are in menopause when you haven’t had a menstrual cycle for 12 months or longer, not due to PCOS or any other cause (secondary amenorrhoea). The diagnosis of menopause is, therefore, retrospective.
You may be in menopause if you haven’t had a cycle for 6 months, but by definition, you are not in menopause because 12 months are not over. This is not just semantics because many women who experience depression, poor sleep, aches and pains, weepiness (and many more) are dismissed as “not in menopause” and therefore do not qualify for hormone therapy.
Perimenopause or menopausal transition
The average age of menopause is 46 to 51 years (depending on your race and ethnicity). Perimenopause, or the menopausal transition, is the 7-8 years before menopause when women may experience changes in menstrual cycles, insomnia, depression, anxiety, hot flashes and many more. Some women may experience perimenopausal symptoms for up to 14 years.
Depression during the menopausal transition
Depression is a mood disorder characterized by persistent sadness, hopelessness, and loss of interest in once-enjoyable activities. It is a common mental health problem that affects people of all ages, genders, and backgrounds.
Difficulty in diagnosing perimenopausal depression
Australian psychiatrist Dr. Jayashree Kulkarni, in a 2018 paper, says
“To complicate matters the physical symptoms of the menopause often present much later (up to five years) than the psychological symptoms. This delay can make the diagnosis of perimenopausal depression very difficult. It is important for health professionals to consider whether women who experience depressive and anxiety symptoms for the first time in their mid-40s are actually experiencing depression related to the perimenopausal hormone fluctuations. Similarly, women who experience an exacerbation of a previously well-controlled depression may also be experiencing a perimenopausal relapse.”
Why are women at a higher risk for depression during the menopausal transition?
Depression during menopause is not just a result of hormonal changes but also due to the psychosocial stressors that may accompany the transition. The menopausal transition is often accompanied by psychosocial stressors, such as aging, changes in social roles, and health concerns, your children may be heading off to study or work outside the home, or you may be in a fulfilling but high-stress job, all of which can contribute to depression.
Hormonal changes during the menopausal transition
You have probably heard of menopause and the menopausal transition as a time of declining estrogen levels. Though estrogen is considered the “big diva” of women’s hormones, several other hormones like progesterone, testosterone, FSH, and LH play essential roles.
The hormonal changes in the perimenopausal period cause changes in the brain that affect mood and emotional well-being.
For some women, perimenopause is a time of complete hormonal chaos, while others may have a smooth ride. As you can see in the image below, estrogen levels may be very high on certain days and low on others. Progesterone levels may be relatively low on days of high estrogen. These fluctuating hormone levels may explain some of the symptoms of perimenopause.
Can hormone therapy during the menopausal transition prevent depression?
In a research paper titled “Efficacy of Transdermal Estradiol and Micronized Progesterone in the Prevention of Depressive Symptoms in the Menopause Transition,” the authors set out to
answer the question of whether estrogen applied on the skin and oral micronized progesterone prevents depression during perimenopause and menopause.
Who was included in the study?
Women, predominantly white, in the age group 45 to 60 years who did not have depression at the time of recruitment to the study. They were followed for 12 months.
What hormones did they receive?
One group of women received patches of 0.1 mg of 17β-estradiol (bioidentical estrogen) and oral micronized progesterone (bioidentical) at 200 mg/d for 12 days of the cycle given every 2 to 3 months. The other group got dummy patches and pills (no hormones).
About the hormones used:
Women in the study were given pharmaceutical bioidentical estrogen and progesterone. Bioidentical means the chemical structure of the hormones used for treatment is the same as what our bodies make.
Transdermal 17 beta-estradiol (estrogen on the skin as a patch or cream) and oral micronized progesterone are very different from the oral conjugated equine estrogens (CEE) and medroxyprogesterone acetate (MPA) that were used in the Women’s Health Initiative (WHI) study, which showed that hormone therapy raised the risks of clotting, heart disease, stroke and breast cancer.
The WHI study (2002) is an observational study that included a large number of women in the age group of 50 to 79 who were on hormone therapy. The hormones used were oral estrogens and medroxyprogesterone acetate, both not bioidentical.
Based on outdated information from the WHI study, well-meaning people, including doctors, have discouraged women from using hormone therapy. This is a great disservice to women.
Hormone therapy today uses transdermal estrogens and oral micronized progesterone, both of which are safe for your heart, brain, mood and breasts. Estrogens on the skin do not increase blood clotting.
Study results: Did hormone therapy prevent depression in the menopausal transition?
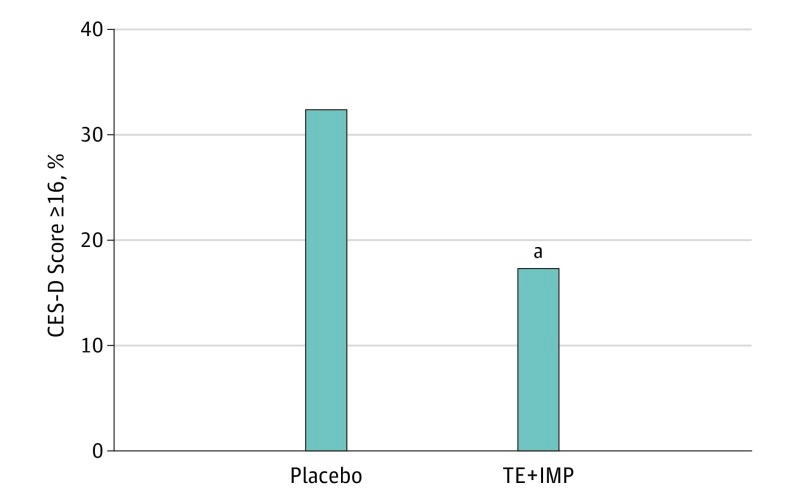
The CES-D score is a measure of depressive symptoms. Placebo includes women who did not receive any hormones, and TE++IMP indicates transdermal estradiol plus intermittent micronized progesterone.
As you can see in the image, women on hormones had a lower depression score. The beneficial effects of hormones were higher in women with high stress levels.
Adverse effects
Some women on hormones had excessive or prolonged menstrual bleeding. There are possibly two reasons for this:
1) Most of the women were in perimenopause-which means they still cycled, and their ovaries still produced some estrogens. Therefore the dosage of estrogen patches could have been high for these women.
2) Progesterone was not given every month. Many doctors think that progesterone should only be used in hormone therapy to prevent uterine cancer to counter the effects of unopposed estrogens. Therefore women who have had a hysterectomy and don’t have a uterus are not prescribed progesterone. But progesterone has multiple benefits on cycle regulation, sleep, anxiety and bones.
The authors wanted to differentiate the effects of estrogen from those of progesterone on depression. They looked at depression scores during the progesterone-free months. Had the women been on progesterone every month, they likely wouldn’t have had excessive bleeding.
BOTTOM LINE
It is encouraging to note that researchers are talking about the prevention of depression. Most often, health professionals talk about treating diseases after they develop.
Multiple studies have shown the benefits of hormone therapy in managing menopausal and perimenopausal symptoms. The correct hormone therapy in women who do not have a recent diagnosis of hormone dependant cancers or severe liver disease is very safe! Accurate information will empower women to make the best treatment decisions. They should not be unduly scared away from hormones.
Besides hormones, psychotherapy, good food, restful sleep, high-quality supplements at therapeutic doses and building stress resilience are equally important. Some women may need antidepressant medications along with hormone therapy and lifestyle changes.
References
- Kulkarni, Jayashri. “Perimenopausal depression–an under-recognised entity.” Australian prescriber 41.6 (2018): 183.
- Gordon, Jennifer L., et al. “Efficacy of transdermal estradiol and micronized progesterone in the prevention of depressive symptoms in the menopause transition: a randomized clinical trial.” JAMA psychiatry 75.2 (2018): 149-157.
- Writing Group for the Women’s Health Initiative Investigators, and Writing Group for the Women’s Health Initiative Investigators. “Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial.” Jama 288.3 (2002): 321-333.