A study recently reported from the Cleveland Clinic in the USA looked at people living with rheumatoid arthritis or psoriatic arthritis.
Rheumatoid arthritis and psoriatic arthritides are chronic inflammatory autoimmune conditions that affect multiple body systems and cause considerable joint pain and low quality of life.
Both these autoimmune conditions do not have a cure at present. Though the recent addition of several DMARDs (Disease-Modifying Antirheumatic Drugs) has given hope to many, not everyone achieves long-term remission.
Moreover, these newer medications can cost a lot of money out of your pocket. In many countries like India, insurance doesn’t cover the cost of medicines used outside the hospital.
Going back to the study, it included about a hundred people, mostly women, in the sixth decade of life, who were under Rheumatologists’ care. They had either rheumatoid arthritis or psoriatic arthritis. All of them received the standard of care as recommended by the American College of Rheumatology.
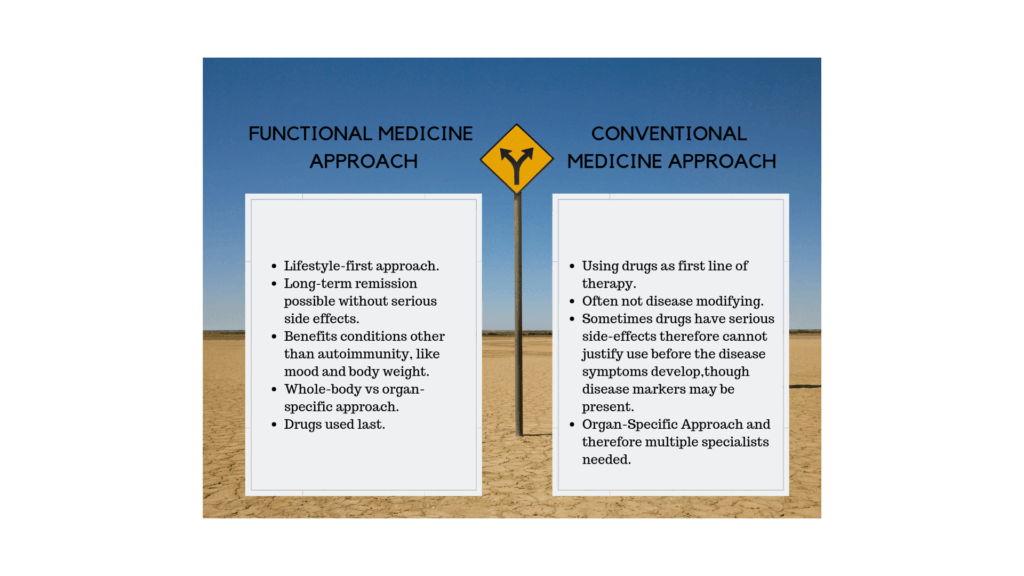
One group of people was under the standard of care, and the other self-selected group was under a Functional Medicine model of care, in addition to guideline-based care.
What did they find?
At the end of 12 weeks, people who used the Functional Medicine model experienced improvements in several parameters compared to those under regular care.
What were the areas of improvement?
People using the Functional Medicine Model experienced:
- Less pain
- Better mental wellbeing
- Better physical health
What did the people in the Functional Medicine group do?
In Functional Medicine, we use food as the first line of therapy. People in this group were encouraged to follow an anti-inflammatory elimination diet.
1) What did they eat?
- Nutrient-dense “real food” and not food that comes from a factory.
- Good fat like avocados, nuts.
- Fish rich in omega 3s.
- Fresh, brightly coloured vegetables rich in phytonutrients (beneficial plants chemicals)
2) What did they avoid eating?
They did not eat gluten, sugar, processed food, dairy.
3) What supplements did they take?
They took supplements based on their advanced laboratory reports. Most commonly, they took supplemental vitamin D3 and Omega 3 fatty acids.
4) What else did they do differently when compared to the standard of care?
They had a team of providers supporting them. Their care teams included a physician or advanced practitioner, registered dietitian and health coach as part of the initial visit and ongoing support. Making lifestyle changes can be challenging at times. Therefore, continued support is crucial in achieving and maintaining good results.
5) How many of them were on medications?
Of the 109 people in the study, 54 people were in the Functional Medicine group and 55 in the standard of care group.
Thirteen people in the Functional Medicine group did not use any medicines because they were not keen to use DMARDs as initial therapy.
All 55 people in the standard of care group were on medications.
Interestingly, disease activity scores were similar, despite the differences in treatment. This means that people who did not take DMARDs were not necessarily worse off. ((Ref))
Bottom line: What does this mean for you?
- Though Rheumatoid Arthritis and Psoriatic arthritis are both chronic long-term painful conditions, it IS possible to get into remission!
- Lower levels of inflammation, being a non-smoker (includes passive smoking), negative rheumatoid antibodies status, no obesity, and sleeping well are important factors.
- Early treatment of RA or PsA can help you achieve remission. Your success is decided by your personal goals and how well you can implement the recommended changes.
- While many of you would prefer a more “natural” approach, for some of you, it may include adding prescription drugs, perhaps at lower doses or if you do not respond adequately to a well-formulated Functional Medicine program.
- A functional medicine model’s success is dependant to a great extent on the type and duration of support available to you.


