Audio summary of the article
Hypertension (high blood pressure) continues to be a critical global health issue, significantly increasing the risk of heart disease, stroke, dementia and kidney failure. As medical knowledge evolves, treatment guidelines and blood pressure targets have also undergone significant changes. This article provides considerations for establishing individualized blood pressure goals, with a particular emphasis on understanding why lower blood pressure numbers are preferable to higher ones.
What blood pressure numbers do current guidelines recommend?
Historically, hypertension guidelines advocated maintaining blood pressure below 140/90 mmHg. However, the 2017 blood pressure guidelines introduced a paradigm shift based on evidence from the SPRINT trial, which enrolled over 9,000 participants without diabetes or a prior history of stroke.
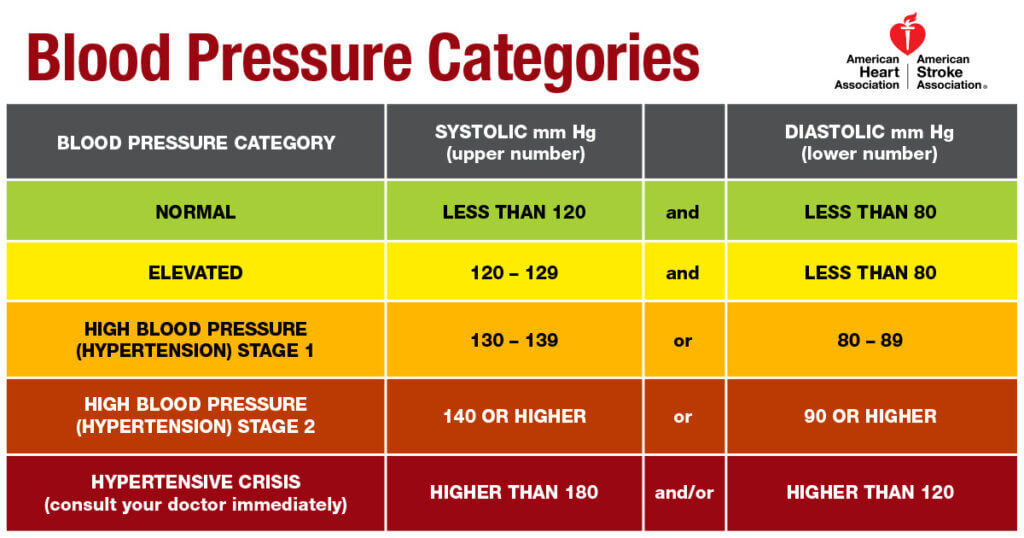
The image below shows the blood pressure categories recommended by the American Heart Association. These categories are generally followed worldwide.
The SPRINT (Systolic Blood Pressure Intervention Trial) found that intensive blood pressure lowering, targeting a systolic blood pressure of less than 120 mmHg, significantly reduced cardiovascular events by 25% compared to standard treatment targeting a systolic blood pressure of less than 140 mmHg. Importantly, the trial also reported a 27% reduction in death from all causes. These impressive results strongly influenced clinical practice, suggesting potential benefits in pursuing more aggressive blood pressure targets.
What about European Blood Pressure guidelines? The 2023 European Society of Hypertension (ESH) and the 2024 European Society of Cardiology (ESC) guidelines continue to define hypertension as blood pressure ≥140/90 mm Hg. However, both sets of guidelines generally recommend treating most adults to achieve a target blood pressure of <130/80 mm Hg, making their treatment recommendations similar to the American guidelines.
While the definition of hypertension and the universal applicability of a systolic blood pressure (SBP) target below 130 mm Hg remain subjects of debate, accumulating evidence indicates that achieving an SBP below 120 mm Hg can substantially reduce heart disease and stroke risks in people at higher risk.
In a recent expert analysis in the American College of Cardiology called Is It Time For a New Blood Pressure Treatment Goal?, the authors briefly discussed several trials and summarized that among people at high risk, treatment to SBP goal <120 mm Hg is beneficial.
Here is a summary of the trials they included:
| Trial | Population | Mean Age | Intensive SBP Target | Standard SBP Target | Major Findings |
|---|---|---|---|---|---|
| SPRINT | Non-diabetic, elevated CV risk | ~68 years | < 120 mm Hg | < 140 mm Hg | ↓Stroke risk: no significant reduction in overall CV events |
| ACCORD | Type 2 diabetes + high CV risk | ~62 years | < 120 mm Hg | < 140 mm Hg | ↓12 % CV events; ↓CV ↓deaths from all causes |
| BPROAD | Type 2 diabetes + HTN | ~63 years | < 120 mm Hg | < 140 mm Hg | ↓21 % major adverse CV events |
| ESPRIT | HTN + high CV risk; included DM/stroke | ~64.6 years | < 120 mm Hg | < 140 mm Hg | ↓12 % CV events; ↓CV ↓deaths from all-causes |
What about people with type 2 diabetes?
While SPRINT provided compelling evidence for lowering blood pressure targets, it did not include people with diabetes. The ACCORD trial filled this knowledge gap by focusing specifically on patients with type 2 diabetes. Over 4,700 participants were enrolled to determine if similarly aggressive blood pressure control (systolic blood pressure <120 mmHg) would yield comparable cardiovascular benefits in diabetic populations.
Unlike the SPRINT trial, the ACCORD study showed mixed outcomes. Intensive blood pressure control reduced the incidence of strokes but did not significantly decrease the overall rate of cardiovascular events. Additionally, intensive management in diabetic patients was associated with higher rates of adverse events, including hypotension, electrolyte disturbances, and acute kidney injury.
However, the more recent BPROAD trial from China that enrolled more than 12,000 participants with diabetes and hypertension to compare similar SBP targets, found a reduced rate of death from cardiovascular causes in the intensive therapy group over 4+ years.
Why is there a difference in the results from the older ACCORD and the newer BPROAD trials?
In an editorial titled, Stratified medicine for blood pressure targets in type 2 diabetes mellitus, the authors explained that BPROAD and ACCORD differed in several important ways. BPROAD, conducted in China (2019–2021), included only Asian participants, whereas the ACCORD trial, done in the USA and Canada (2003–2005), mostly comprised White and Black people. Because BPROAD was more recent, about 25% of participants were already using newer diabetes medications, such as SGLT2 inhibitors (which protect the heart and kidneys), DPP-4 inhibitors, and GLP-1 receptor agonists (used for weight loss). Fewer blood pressure medications were needed in BPROAD than in ACCORD-about 2.2 versus 3.4 drugs in the intensive groups and 1.4 versus 2.1 in the standard groups.
Given the wide variations in heart disease and stroke risks in different populations, blood pressure targets need to be individualized.
Balancing Benefits and Risks in Intensive Blood Pressure Management
In the SPRINT trial, participants in the intensive treatment arm required an average of approximately 2.8 medications (often rounded to 3), while those in the BPROAD trial required about 2.2 medications in the intensive arm. In practice, most patients need two to three antihypertensive agents to reach target blood pressure, and intensive lowering typically adds about one additional medication on average. It is worth noting that the BPROAD population required fewer medications than the SPRINT population, likely because a significant proportion of participants were also on weight–loss–promoting therapies, such as GLP-1 receptor agonists, which are known to lower blood pressure. This likely contributed to the reduced medication burden observed in BPROAD.
More medications, higher potential for side effects: One consistent observation from intensive blood pressure management studies shows that while cardiovascular benefits exist, risks such as dizziness, syncope, electrolyte disturbances, renal impairment, and falls significantly increase. These risks are particularly pronounced in older adults or individuals with multiple comorbidities, underscoring the importance of individualized blood pressure targets tailored to patient-specific health conditions, age, and overall treatment tolerance.
What about blood pressure targets in women?
Studies have shown that women need a lower blood pressure target than men.
Read What is normal blood pressure for women?
Future Perspectives: Combining Lifestyle Change and Medications
One area where the evidence remains limited is the role of combining structured lifestyle interventions with prescription medications in achieving lower blood pressure targets. While major trials, such as SPRINT, ACCORD, BPROAD, and ESPRIT, demonstrated the cardiovascular benefits of intensive blood pressure lowering through medication titration, none formally tested whether structured lifestyle changes, alongside medications, improve outcomes beyond standard advice. Smaller trials, including PREMIER, TONE, and DASH-Sodium, have clearly shown that structured lifestyle changes—such as sodium restriction, weight loss, and the DASH diet or a low-carbohydrate diet—can significantly lower blood pressure and sometimes reduce the need for medication. However, no large randomized controlled trial has yet evaluated whether an integrated approach of intensive pharmacologic treatment combined with intensive lifestyle change reduces cardiovascular events more effectively than medications alone.
The evolving landscape of hypertension management, shaped by groundbreaking research, highlights the complexity and necessity of personalized treatment approaches. Achieving lower blood pressure targets can significantly reduce cardiovascular risk but requires careful, individualized planning and monitoring.
References:
- SPRINT Research Group. “A randomized trial of intensive versus standard blood-pressure control.” New England Journal of Medicine 373.22 (2015): 2103-2116.
- ACCORD Study Group. “Effects of intensive blood-pressure control in type 2 diabetes mellitus.” New England Journal of Medicine 362.17 (2010): 1575-1585.
- Liu J, Li Y, Ge J, et al. Lowering systolic blood pressure to less than 120 mm Hg versus less than 140 mm Hg in patients with high cardiovascular risk with and without diabetes or previous stroke: an open-label, blinded-outcome, randomised trial. Lancet. 2024;404(10449):245-255. doi:10.1016/S0140-6736(24)01028-6
- Li, J., J. Liu, and ESPRIT Collaborative Group. “Effects of intensive blood pressure lowering treatment in reducing risk of cardiovascular events.” Circulation 148 (2023): e282-e317.
- Bi, Yufang, et al. “Intensive blood-pressure control in patients with type 2 diabetes.” New England Journal of Medicine 392.12 (2025): 1155-1167.
- Fernandez-Fernandez, Beatriz, et al. “Stratified medicine for blood pressure targets in type 2 diabetes mellitus.” Nephrology Dialysis Transplantation (2025): gfaf007.
- Saslow, Laura R., et al. “Comparing very low-carbohydrate vs DASH diets for overweight or obese adults with hypertension and prediabetes or type 2 diabetes: A randomized trial.” The Annals of Family Medicine 21.3 (2023): 256-263.
- Craddick, Shirley R., et al. “The DASH diet and blood pressure.” Current atherosclerosis reports 5 (2003): 484-491.
- Writing Group of the PREMIER Collaborative Research Group. “Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial.” Jama 289.16 (2003): 2083-2093.
- Whelton, Paul K., et al. “Sodium reduction and weight loss in the treatment of hypertension in older persons: a randomized controlled trial of nonpharmacologic interventions in the elderly (TONE).” Jama 279.11 (1998): 839-846.